The 2010 Affordable Care Act (or ACA, widely nicknamed “Obamacare”) sought to expand health insurance coverage via a variety of methods, among them a dramatic expansion of Medicaid, the joint federal-state insurance program primarily serving low-income Americans. In a study we just published with the Mercatus Center at George Mason University, we found that expansion has come with an apparent cost: specifically, shifting Medicaid program resources away from low-income children.
Understanding this requires some familiarity with Medicaid and its recent expansion. Historically, Medicaid has provided health insurance coverage for certain low-income individuals, including children, pregnant women, parents and caretakers, as well as for aged and disabled Americans who were eligible for other forms of federal income assistance. The ACA sought to expand Medicaid coverage to include non-aged, non-disabled childless adults with incomes ranging up to 138% of the federal poverty line.
Though the ACA as originally enacted sought to make this Medicaid expansion mandatory, a 2012 Supreme Court decision rendered expansion optional for states. As a result, some states expanded Medicaid immediately on the earliest possible date of January 1, 2014, some expanded only later, and some have still not expanded. As of this writing, 39 states plus the District of Columbia have elected to expand, while 11 states, including North Carolina, have not.
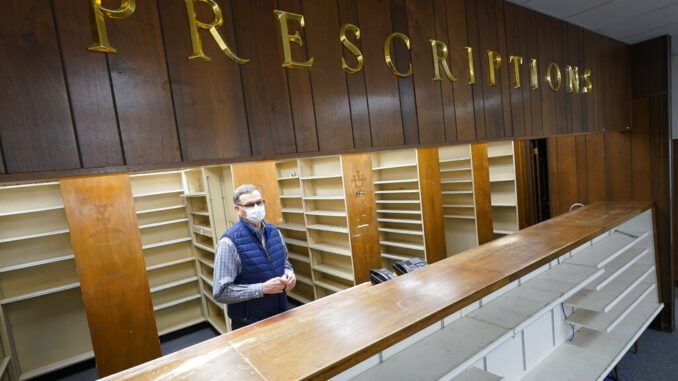
Medicaid expansion under the ACA facilitated a dramatic increase in program enrollment. Today approximately 22% of all Medicaid enrollees under the age of 65 are enrolled because of the ACA. However, there has been no commensurate increase in the suppliers of Medicaid services. For example, only about 74% of physicians accepted Medicaid in the years following expansion, nearly the same percentage as before expansion.
With a much greater demand chasing a limited supply of Medicaid services, something had to give. That something, apparently, is the share of program resources allocated to health care for children.
In states that chose to forego expansion, there has been a remarkable consistency in the distribution of Medicaid spending. In these non-expansion states, the shares of program resources allocated respectively to children, the aged, the disabled, and to non-aged, non-disabled adults, were all almost exactly the same in 2019 as in 2013. Anywhere expansion has not been a factor, spending on each group has risen steadily and proportionally.
In expansion states, however, the situation has been quite different. These states have shifted Medicaid financial resources away from low-income children toward the non-aged, non-disabled adults who were the focus of expansion and for whom the federal government provides a much higher reimbursement rate.
In states that expanded in January 2014, per capita Medicaid spending on children was only 5.9% higher in 2019 than it was in 2013. That’s an annual increase of less than 1% per year. Contrast that with the 22.7% growth in per capita Medicaid spending on children in non-expansion states, or with the 27.0% growth in average per capita personal health care expenditures nationally, from 2013 to 2019. Per capita Medicaid spending on children in expansion states has grown less than one-third as fast as health spending has elsewhere.
We found other shifts in spending within expansion states, including slower growth of per capita spending on older or disabled adults coupled with faster growth of spending on younger, non-disabled adults. However, these shifts were smaller and less definitive than the striking differences with respect to children.
We stress that we do not know the reasons for these shifts in Medicaid resources. Nor can we say whether the shift in Medicaid’s financial resources has been accompanied by an equal shift in access to care. All we are able to say based on our own research is that children are receiving a much smaller share of Medicaid resources in expansion states than they were before expansion, and that we don’t see this pattern in states that opted not to expand Medicaid.
The history of federal policymaking is quite often a history of unintended consequences. The lawmakers who enacted the ACA clearly did not intend to shift Medicaid resources away from low-income children in the process of bringing millions of relatively higher-income childless adults onto the Medicaid rolls.
However, that’s what has happened in states that expanded Medicaid.
Whenever changes to Medicaid’s eligibility rules are considered, whether it’s a possible future expansion of Medicaid or a reconsideration of a recent expansion, it’s important to understand their effects on vulnerable Americans. Low-income children seem especially deserving of such consideration.
Charles Blahous is senior research strategist and Liam Sigaud is a research assistant with the Mercatus Center at George Mason University.